WHAT IS DIABETES?
Diabetes mellitus is a condition associated with blood sugar (glucose) level in the blood being too high (known as hyperglycaemia). This can occur in early life (1st or 2nd decade, often referred to as type 1 diabetes) or later in life (middle to late age, often referred to as type 2 diabetes). The cause for both conditions developing is unknown though there are genetic and immune system factors that play a role. In type 1 diabetes, the pancreas doesn’t produce enough insulin (the hormone that helps to reduce blood glucose levels). For type 2 diabetes, it is often related to being overweight and there being an intolerance to the normal action of insulin.
HOW DOES IT AFFECT THE EYE?
Diabetes damages both large and small blood vessels throughout the body. It is the damage to the small blood vessels (microvascular disease) that is of particular relevance to the eye, as all the blood vessels that supply the eye are small. As a result of long-term hyperglycaemia, two changes occur in small blood vessels:
(a) The very small blood vessels (known as capillaries) normally have a thin basement membrane around a single layer of cells (endothelial cells). This basement membrane becomes thickened in diabetics, and as a result the vessels themselves become narrowed.
As a result of the vessels becoming narrowed, there is not enough blood supply reaching the retinal tissue and the retina becomes “hypoxic” (hypoxic = lacking in oxygen supply). Thus, the retina responds by producing molecules that stimulate the formation of new blood vessels (so called neovascularisation). Whilst intuitively one might think this was a sensible solution to the lack of blood supply to the retina, the problem lies in the nature of these “new” blood vessels. They are often very leaky (see point (b) above) and bleed easily. After bleeding, the vessels contract and can pull on the retina causing a so-called “tractional retinal detachment”. This is a different entity from the retinal detachment caused by a retinal tear. Thus narrowed retinal blood vessels at the back of the eye can ultimately lead to two problems, haemorrhage into the cavity of the eye (vitreous haemorrhage) and tractional retinal detachment. Both these conditions may result on reduced vision.
(b) The blood vessels of the retina have a very special property (which they share with the blood vessels of the brain), i.e. they have a “barrier” function, which prevents fluid and large molecules “leaking” from the vessel into the surrounding tissues. Hyperglycaemia results in damage to these cells that maintain this normal “barrier” function, and as a result the blood vessels become leaky.
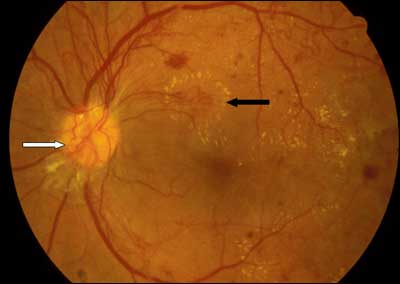
As a result of the vessels becoming “leaky”, fluid can accumulate over the central part of the retina (the macula). The central macula is the thinnest part of the retina because it is the area of retina that provides us with our high-level of vision in the centre. This is the part of the retina that we use when we are reading, or watching TV, or looking at people’s faces. Thinness of this structure helps to reduce light scatter and therefore if the tissue is “water-logged” with fluid (as can happen in diabetics), vision can be reduced as a result (the technical term for this is macular oedema – literally fluid at the central retina). The image below shows an eye with diabetic retinopathy. the white arrow points to the "new" blood vessels arising because of poor blood supply to the back of the eye. The black arrow shows an area of whitening related to "leaky" blood vessels.
HOW CAN IT BE TREATED?
The most important factor in controlling diabetic retinopathy is controlling your blood sugar control long-term, in addition to controlling other cardiovascular risk factors, such as blood pressure, cholesterol, not smoking, etc. Your physician and/or general practitioner have a crucial role to play in this regard. However despite this, many individuals still progress to develop sight-threatening diabetic retinopathy. The mainstay of treatment for sight-threatening diabetic retinopathy is laser treatment. This is very different to laser treatment that is given to individuals who wish to get rid of their glasses. The laser treatment for diabetic retinopathy involves creating laser scars on the retina, which depending on the type of laser treatment will alter the retinal haemodynamics and improve the condition.
WHAT IS THE ROLE FOR SURGERY?
There are three main indications for vitreoretinal surgery in diabetics. All of them relate to the complication of retinal blood vessels becoming narrowed, and new blood vessels occurring as a result.
(a) Vitreal haemorrhage: If the new blood vessels bleed, they may fill the cavity of the eye (the vitreous chamber) with blood. In the majority of cases this blood will resolve by itself. However, on occasion the blood does not clear by itself and persists. In this circumstance, it may be desirable to do an operation to clear the blood (so-called vitrectomy), especially if there is the need to perform further laser treatment and the presence of the blood prevents the surgeon getting a view of the retina in order to do the laser treatment.
(b) Recurrent vitreal haemorrhage: In this scenario, the bleed is exactly the same as in (a) but though it clears, the patient may get recurrent frequent bleeds. Examination of the retina may reveal an area of traction with associated retinal blood vessels that recurrently bleed due to this traction. Often the only mechanism that can relieve this traction is an operation (again a vitrectomy).
(c) Finally, the retina may be detached as a result of contraction of the new blood vessels pulling on the retina. This may or may not also be associated with a tear in the retina. If the detachment involves the center part of the retina (macula), this will usually require surgery.
Retinal surgery for diabetics is termed a “diabetic vitrectomy”. The surgery can usually be done either under local or general anaesthetic. Three small “key-hole” incisions are made through the coat of the eye, and the surgeon removes the vitreous gel (and associated haemorrhage). The gel is replaced with the clear fluid that fills the front of the eye (aqueous). In addition to removing the vitreous, the surgeon may also perform more laser to the retina and occasionally a gas bubble (very rarely an oil bubble) may be used. If a gas bubble is used, the patient cannot fly until the gas bubble dissolves by itself (usually 4 to 8 weeks).
As a vitreoretinal surgeon, Niall Patton has particular expertise in diabetic eye disease, both in the medical management (including laser treatment) and surgery. To organise an appointment, contact his secretary, or fill in the contact form.