IMPORTANT
Retinal detachment is often an emergency. It is imperative that if you have any of the symptoms below, that you be seen promptly. Either contact your local Accident & Emergency service, or your local Ophthalmic Service. Niall Patton can arrange urgent reviews as a private patient out-of-hours.WHAT IS IT?
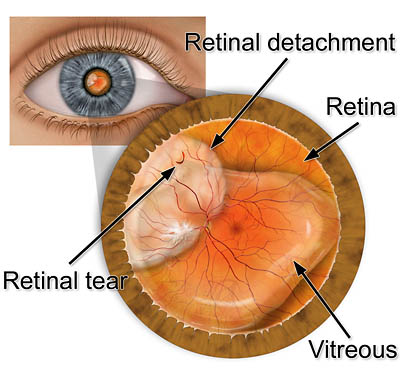
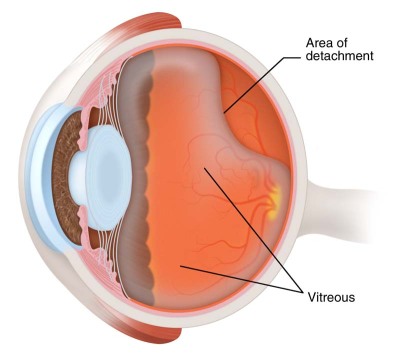
A retinal detachment is a condition where the retina at the back of the eye "detaches" from its normal position. An analogy is of wallpaper stripping off a wall. If we imagine the eye to function in a similar way as a camera, the retina represents the "film" at the back. Images strike the retina which then sends the images to the brain for processing, which results in what we know as the sense of sight. If the retina is not in the correct position, it will not function properly and sight will be affected.
WHO GETS IT?
The most common mechanism for retinal detachment is related to the vitreous (sometimes referred to as vitreous gel) at the back of the eye. The vitreous fills the cavity at the back of the eye, and is normally attached to the retina. If the vitreous detaches from the back of the eye, it can pull on the retina and cause a retinal tear. This tear can then proceed to cause the retina to detach, and move away from its normal position. The causes for the vitreous to detach are unknown, but risk factors including getting older, being short-sighted (myopic) and trauma (physical injury).
WHAT ARE THE SYMPTOMS?
Symptoms commonly reported relating to the vitreous detaching are flashing lights and floaters. Those having a retinal tear also often report these, as the mechanism is the same in both. If a tear proceeds to a retinal detachment, in addition to experiencing flashing lights and floaters, patients often experience a shadow in their vision. This shadow corresponds to where the retina has detached and serves as a good clue as to which part of the retina (e.g. the upper or lower) has detached. Finally, the patient with a retinal detachment may also experience loss of central vision. This is an important sign, as it often indicates the retina has detached in the centre (the centre of the retina is called the macula).
HOW IS IT TREATED?
If a retinal detachment is not treated promptly, it will often lead to permanent visual loss. The degree of how urgent an operation needs to be performed will depend on several factors, the most important of which is whether the centre of the retina (the macula) is still attached or not. If the macula is attached, then prompt surgery may prevent the development of significant visual loss. If however the macula is detached at the time of surgery, whilst the operation can still restore vision to the eye, the ultimate vision that can be achieved will be limited and it is likely that vision may never return to what it once was in that particular eye. However without surgery, the prognosis is very poor and a large number of untreated retinal detachments may go blind in the untreated eye.
WHAT DOES THE SURGERY INVOLVE?
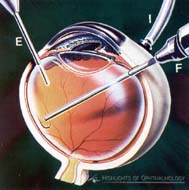
The surgery can be done with the patient either awake (local anaesthesia) or asleep (general anaesthesia). In certain circumstances, your surgeon will guide you as to the most appropriate anaesthesia for your eye. There are two main techniques used to reattach the retina. The most commonly performed operation is called a vitrectomy and involves a “keyhole” procedure, with three small incisions made through the coat of the eye. The aim of the procedure is to remove the source of the traction (the vitreous gel) that caused the tear(s) in the first place. After the gel is removed (replaced by a saline infusion), the retina is put back into place using a gas bubble. In certain circumstances, the surgeon may opt to use an oil bubble instead of gas. Finally, the surgeon “seals” the retinal tears using either laser or cryotherapy (freezing treatment). This is analogous to “spot-welding” the tear closed, so that when the gas dissolves (usually 4-8 weeks), the tear is sealed and the retinal detachment is repaired. It is important to note that if you do have gas in your eye, you will have very poor vision in the eye until the gas dissolves, and that you cannot fly in an aeroplane until the gas dissolves. The other established technique to repair a retinal detachment involves placing a piece of silicone material (called a buckle) to the coat of the eye and treating the retinal tears with cryotherapy. This procedure would normally have to be done under general anaesthetic and is appropriate for certain retinal detachments, depending on the particular clinical features in any individual case.
HOW SUCCESSFUL IS THE SURGERY?
In terms of getting the retina back in place, success of retinal detachment surgery tends to be approximately 80-90% with one operation. This means approximately 10-20% will require more than one operation. Those less likely to be successful with one operation include those whose retina has been detached for a long period of time before surgery, where the retina may be scarred. In terms of final level of vision, as stated earlier, the most important factor is whether the retina in the centre (the macula) is affected (ie detached) prior to surgery.